Abstract
The objective of this investigation is to review existing research pertaining to cognitive impairment and decline following critical illness and describe a case involving a 49-year-old female with sepsis and acute respiratory distress syndrome (ARDS) with no prior neurologic history who, compared to baseline neuropsychological test data, experienced dramatic cognitive decline and brain atrophy following treatment in the medical intensive care unit (ICU) at Vanderbilt University Medical Center. The patient participated in detailed clinical interviews and underwent comprehensive neuropsychological testing and neurological magnetic resonance imaging (MRI) at approximately 8 months and 3.5 years after ICU discharge. Compared to pre-ICU baseline test data, her intellectual function declined approximately 2 standard deviations from 139 to 106 (from the 99th to the 61stpercentile) on a standardized intelligence test 8 months post-discharge, with little subsequent improvement. Initial diffusion tensor brain magnetic resonance imaging (DT-MRI) at the end of ICU hospitalization showed diffuse abnormal hyperintense areas involving predominately white matter in both hemispheres and the left cerebellum. A brain MRI nearly 4 years after ICU discharge demonstrated interval development of profound and generalized atrophy with sulcal widening and ventricular enlargement. The magnitude of cognitive decline experienced by ICU survivors is difficult to quantify due to the unavailability of pre-morbid neuropsychological data. The current case, conducted on a patient with baseline neuropsychological data, illustrates the trajectory of decline occurring after critical illness and ICU-associated brain injury with marked atrophy and concomitant cognitive impairments.
Keywords: ARDS, brain injury, critical care, executive dysfunction, sepsis
Review of Cognitive Functioning in Survivors of Critical Illness
The primary outcomes of interest following critical illness, defined as illness requiring treatment in the intensive care unit (ICU), have traditionally been mortality and morbidity. However, recent advances in technology and medicine have significantly reduced mortality rates1 and extended the lives of the critically ill, thus shifting concerns from survival to preservation of quality of life and emotional and cognitive functioning–domains threatened and potentially comprised by the effects of critical illness. Such concerns are well-founded, particularly as they relate to cognitive abilities which are highly vulnerable due to ICU-related insults2,3 and are vital to the well-being and functional outcomes of ICU survivors.
While research is, in many respects, in its infancy, evidence from over a dozen epidemiologic investigations (totaling approximately 500 subjects) suggests that over 50% of ICU survivors may experience significant and persistent cognitive impairment, widely referred to as long-term cognitive impairment (LTCI).4–9 The impairment occurs in wide-ranging domains including executive functioning, memory, attention, visual-spatial construction, language, and other areas.7,10,11 In general, impairment ranges in severity from mild to very pronounced and is often sufficiently disabling enough to effect quality of life and the ability to return to work.5–7 Patients appear to be susceptible to the development of cognitive impairment regardless of age, level of education, or severity of illness.2,7However, virtually all investigations conducted to date have been done with relatively young subjects (mean age 54 years), so the degree to which advanced age is a risk factor for the development of impairment remains largely unknown. As is true following most kinds of brain injury, partial recovery of functioning occurs over time, with patients rarely returning to premorbid baselines.3 Among those with pre-existing early forms of neurodegenerative disease such as mild cognitive impairment (MCI), critical illness may amplify and accelerate the descent into frank dementia, as has been shown in animal models.12
Potential contributors to cognitive decline in ICU survivors have not been widely studied and, in light of the highly heterogeneous nature of critical illness, there is almost certainly no single explanation for the neuropsychological impairment experienced by these individuals.11 Biologically plausible mechanisms which are increasingly the focus of attention include delirium, inflammation, and others.13,14 Delirium occurs in up to 80% of ICU patients15,16 and appears to be associated with hypoperfusion in frontal, temporal, and subcortical brain regions (susceptible to even slight alterations in blood flood), thus leading to the development of neuropsychological deficits.17–19 Inflammation is associated with a wide array of conditions resulting in critical illness; inflammation occurs in all patients with septic shock, sepsis, and acute respiratory distress syndrome (ARDS) and has clear negative implications for the brain.20,21 Inflammatory responses are mediated by cytokines that penetrate the blood-brain barrier and directly or indirectly modulate brain activity, potentially altering neurotransmission22 and presumably worsening cognitive impairment or contributing to new cognitive impairment.
Although a consensus is emerging among clinicians and researchers regarding the long-term effects of critical illness on cognitive functioning, little if anything is known regarding the precise magnitude of cognitive decline in ICU survivors. In the case of individuals undergoing a transplant or an elective surgical procedure (e.g., cardiac surgery), neuropsychological testing is often done prior to hospital admission in order to accurately quantify baseline cognitive functioning and to determine the degree of change following surgery.23–26Medical ICU admissions are not elective as they typically occur due to rapidly developing conditions such as pneumonia, sepsis, or ARDS; as such, it is nearly impossible to precisely determine baseline levels of cognitive functioning in patients with such conditions. No such baseline data exist among medical ICU cohorts, as comprehensive baseline neuropsychological test data is nonexistent among all of the roughly 500 participants in the aforementioned studies, as it is not possible to determine who will develop a critical illness.
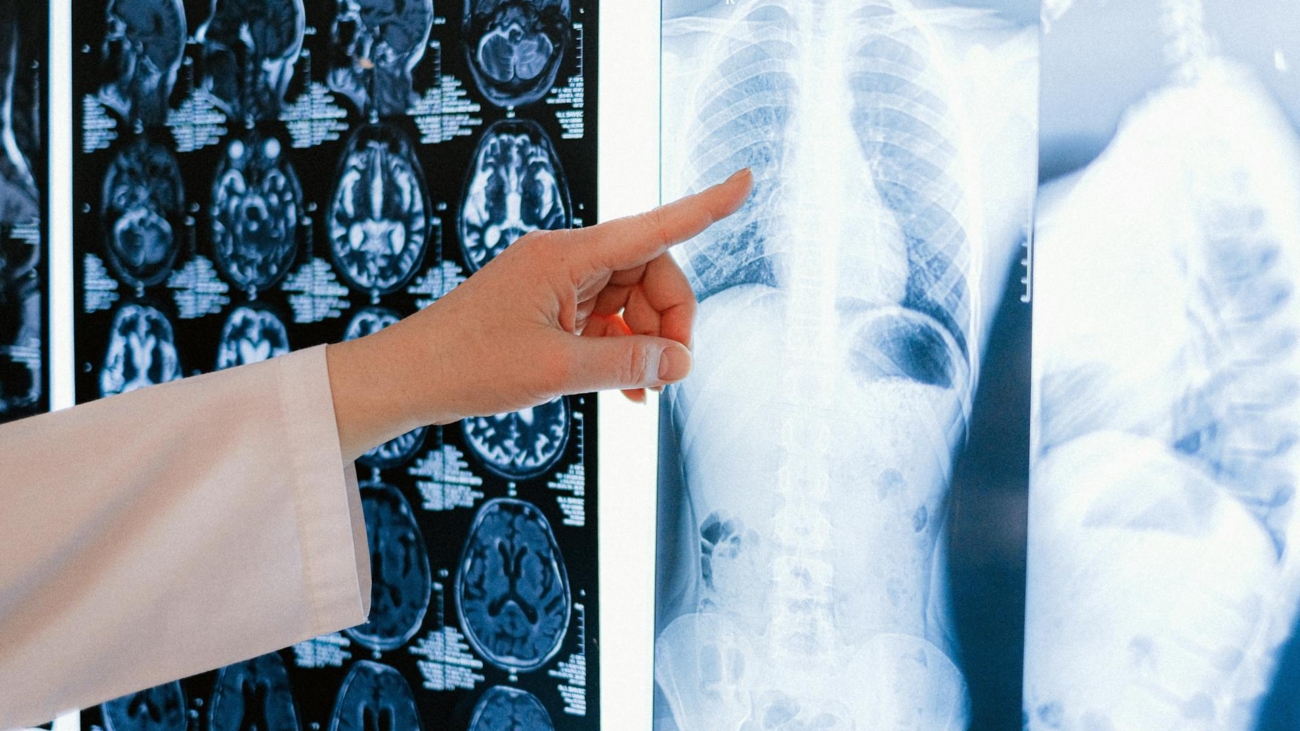
We present a case that is both novel and unique relative to available literature involving a 49-year-old survivor of sepsis and ARDS in whom we were able to quantify the degree of intellectual and cognitive decline due to the presence of previous neuropsychological test data. She underwent IQ testing at 32 years of age and, following her critical illness, she was retested with a revised version of the same IQ instrument [Wechsler Adult Intelligence Scale-III (WAIS-III)] while undergoing comprehensive neuropsychological testing and structural brain MRI. Further, we documented neuropathologic changes both initially and longitudinally on brain MRI scans.
Materials and Methods
The patient participated in detailed clinical interviews and underwent comprehensive neuropsychological testing and neuroimaging (MRI) at approximately 8 months and 3.5 years after ICU discharge. Her inpatient hospital medical records were reviewed. Institutional Review Board (IRB) approval was obtained from the Vanderbilt University IRB, and written consent was obtained from the patient to publish the findings presented herein.
Results
Clinical Course
History of illness
Following a 9-day history of sore throat, fevers, chills, nausea, vomiting, and productive cough with presyncope, this 49-year-old female with a history of mild asthma and hypertension, but no neurologic history, presented to a local community hospital with community-acquired pneumonia. Despite 5 days of intravenous antibiotics, her condition progressed to severe sepsis that necessitated transfer to the Vanderbilt University Medical Center ICU. Upon arrival at the ICU, the subject was profoundly hypoxic and hypotensive and required immediate intubation, mechanical ventilation, and vasopressor support (Table 1shows her medical data). Bilateral lung lower lobe infiltrates without pleural effusions were found on chest radiographs, consistent with the diagnosis of ARDS. She became septic and progressed to septic shock. After approximately 3 weeks of aggressive medical care in the ICU, her clinical course began to improve slowly. She was successfully extubated on day 36 and was transferred to the general medical unit on day 37. Thereafter, she was discharged to local rehabilitation, with a total hospital length of stay of 43 days.
Discussion
The present case involves a critically ill 49-year-old female (49 years old at the time of ICU admission) with a minimal prior medical history and no pre-existing cognitive impairment who developed sepsis and ARDS but who did not experience frank neurologic insults during the course of her critical illness. Her case demonstrates the profound impact of critical illness on long-term neurocognitive functioning and brain integrity and the magnitude of cognitive decline. Although several cohort studies have reported a high prevalence of cognitive impairment in ICU survivors8,33,6 none have had available premorbid neuropsychological data with which to compare postcritical illness performance. Therefore, to our knowledge, this is the first investigation to objectively quantify the extent of cognitive decline after an ICU hospitalization compared to premorbid neuropsychological data.
Our patient had an initial decline in intelligence of approximately 2 SD on measures of verbal, performance, and full-scale intelligence after hospital discharge–a decline from >99th to the 61st percentile. This decline is remarkable as it is significantly larger than the decline observed among patients after cardiopulmonary bypass surgery and other serious medical procedures or illnesses.34–37 Along with a pattern of global intellectual decline, the patient had mild impairments in attention and visual memory and significant impairment in executive functioning. Her executive functioning difficulties were particularly notable in light of both their severity and their correspondence with subjective complaints of deficits in planning and problem solving. If an individual with average intellectual abilities at baseline (IQ of 100, 34th percentile) experienced the precipitous decline observed in our patient, he or she would function at a level consistent with a diagnosis of mild mental retardation (IQ of 70, 2nd percentile). Concomitant with her decline in cognitive function are the neuroimaging findings that show initial significant signal abnormalities in white matter and specific structures such as the hippocampus, a critical structure for memory. These findings likely reflect brain injury due to critical illness with sepsis and ARDS and its treatment. Such findings have been unreported to this point and supplement existing data regarding brain imaging abnormalities in ARDS survivors.38,39
At the time of her second follow-up evaluation (3.5 years after ICU discharge), she continued to report the presence of neuropsychological difficulties severe enough to negatively impact her daily functioning. She demonstrated executive dysfunction, displayed cognitive abilities far below her pre-ICU baseline, and manifested a variable neuropsychological profile by both slight improvement and slight decline. The persistent, and likely permanent, cognitive impairments experienced by the patient are supported by significant brain atrophy and ventricular enlargement (Fig. 3, Table 3).
Although the etiology of her cognitive dysfunction is unknown, it is likely multi-factorial. Possible contributors include delirium40,41 and sepsis-related inflammation, as well as hypoxia4 and glucose dysregulation.42 Inflammation in the brain results in the activation of microglial cells that function as “scavengers” and eliminate dead or injured neurons.20–22Animal models have demonstrated learning and memory impairment as well as executive dysfunction following sepsis,43,44 and Hopkins et al4,8 reported that a majority of survivors of ARDS, itself characterized by severe inflammation, have persistent cognitive impairment after discharge. As noted in the introduction, delirium, which occurred in varying manifestations in our patient for almost 2 weeks, may be associated with cerebral hypoperfusion in subcortical regions populated by structures exquisitely sensitive to slight blood flow changes.17,18 Evidence from clinical investigations suggests that executive dysfunction, as well as other forms of impairment, commonly develops secondary to reduced blood flow to vulnerable subcortical structures, even in the absence of frank ischemic injury.19
While the precise cause of her intellectual decline and ongoing executive function and memory deficits remains unclear, it seems very likely that these difficulties are the result of events associated with her critical illness and/or its treatment. This conclusion is bolstered by her history of robust premorbid functioning; the absence of learning disabilities, prior brain injury, cardiac disease, meningitis, psychiatric or neurologic disorders; and her relatively young age—all factors inconsistent with dementia or other insidious etiologies of cognitive impairment. Although her intellectual functioning was assessed 17 years prior to her ICU admission, it is unlikely that her scores would have changed significantly insofar as IQ scores (particularly composite scores) are typically stable across time and do not significantly decline between young adulthood and middle age.45–47
Conclusion
The cognitive impairments and intellectual decline experienced by our subject 3.5 years following ICU discharge— and concomitant significant brain atrophy and ventricular enlargement—appear to be related to the effects of her critical illness with sepsis and ARDS. This decline resulted in a clinically significant disruption to her overall functioning and led to difficulties with organization, multitasking and efficiency. That the striking decline from premorbid to postcritical illness IQ scores mirrors the interval development of marked atrophy on brain imaging (computed tomography and MRI) suggests a potential mechanistic role of neuronal loss in the development of cognitive impairment. Whether the primary contributors to her cognitive dysfunction and brain atrophy are delirium, the toxic effects of sepsis on the brain, the sedative medications used while on the ventilator, hypoxia, or some other etiology is unclear. Nonetheless, this case raises awareness of the brain injury and concomitant cognitive decline following critical illness and highlights a number of key clinical and research-related implications. Notably, this case demonstrates that cognitive decline can be profound even in middle-aged and robustly healthy ICU patients who, in the context of their critical illness, do not experience frank neurologic traumas or insults. Such a finding is important because individual physicians and medical teams may be relatively less attuned to the needs of these patients than to frail or elderly ICU survivors or those with obvious forms of cognitive impairment. Further, it suggests that cognitive impairment in survivors of ARDS and sepsis may include memory and executive dysfunction—an important insight as this kind of impairment involves a disruption of abilities such as planning and organizing and, as such, may be particularly detrimental to daily functioning. Finally, it points to the need for further research focusing on issues including more fully identifying cognitive impairment associated with ARDS and sepsis, identifying modifiable risk factors that contribute to such impairment, and beginning to pilot the development of ICU follow-up clinics which could facilitate routine neuropsychological screening and psychological intervention to survivors of critical illness at high risk for cognitive decline.